
Expertise
Our ambition is to become the first laboratory to market a intraoperative autotransfusion system capable to wash and recover both red blood cells and platelets during hemorrhagic surgery, using equipment that is ergonomic and intuitive.
To this end, we work closely with teams of reference anesthetists and resuscitation specialists with the aim of improving patient benefits, simplifying the work of physicians and helping to reduce healthcare costs.
Why look for an alternative to standard blood transfusions?
In France, more than 500,000 persons receive a blood transfusion each year. Although necessary and potentially life-saving, allogeneic blood transfusions must nevertheless be justified.
Transfusions are frequently used during highly hemorrhagic surgery, or in situations of absolute emergency.
But transfusions are not without risks.

Persons undergo a transfusion in France each year. Although necessary and potentially life-saving, allogeneic blood transfusions must nevertheless be justified.
According to Dr. Aryeh Shander, up to 60% of allogeneic transfusions could be considered inappropriate, increasing multiple risks. Autotransfusion reduces these risks and may also help preserve banked blood supplies.
The number of haemovigilance declarations made to the French Health Authority (“HAS”) in 2018
All risks are increased with the transfusion of allogeneic platelets.
The maximum number of days of storage for allogeneic platelet concentrates.
Direct and indirect incremental costs of acquiring a unit of allogeneic transfusion product compared with implementing intraoperative blood recovery.
For all these reasons, since 2010, health authorities or public health organizations have been recommending to limit the transfusion of donor blood and to prefer alternatives such as autotransfusion or intraoperative blood recovery.
Since 2010, the World Health Organization and Patient Blood Management have been promoting the use of autotransfusion, both in the interest of the patient and to reduce healthcare costs.
Over the past 10 years, many studies have shown a sharp decrease in healthcare costs achieved by applying these guidelines.

Autotransfusion or Intraoperative Cell Salvage (IOCS):
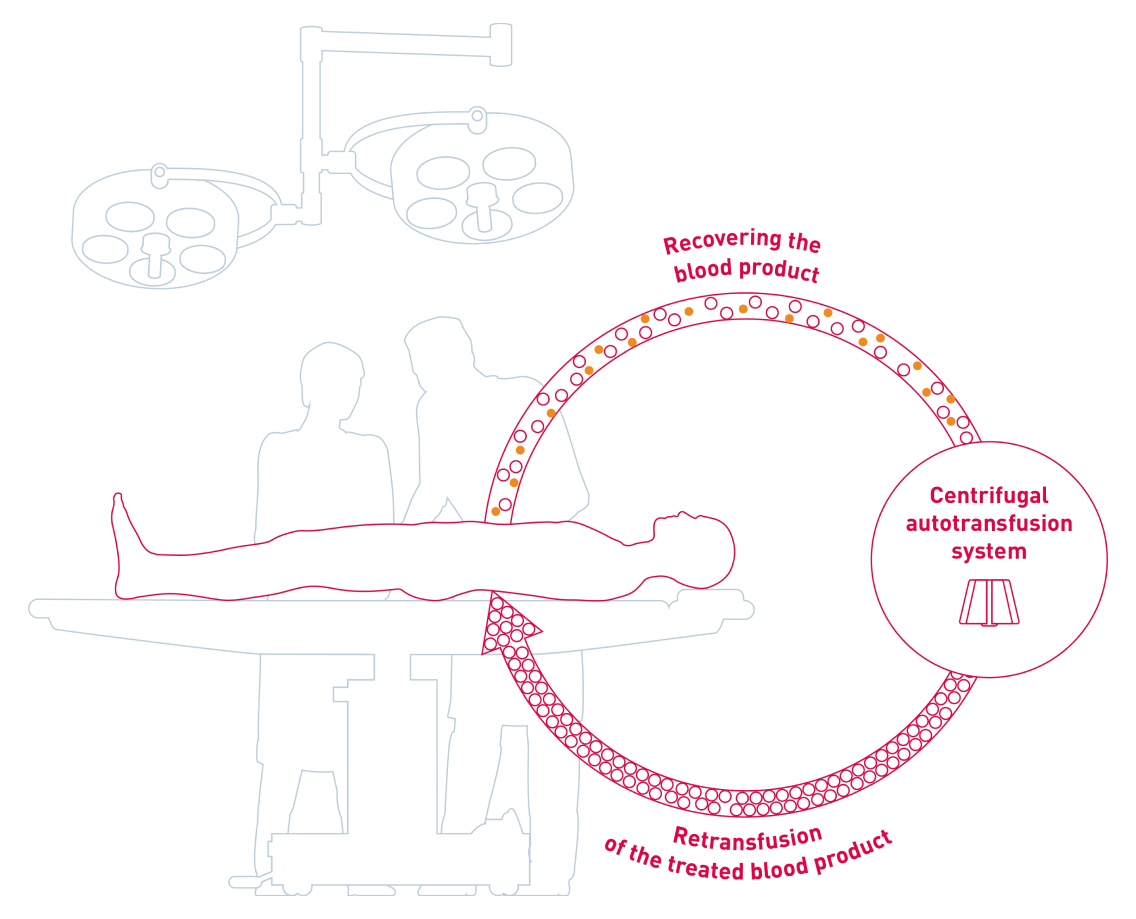
Intraoperative autotransfusion aims to collect blood lost by the patient during hemorrhagic surgery to treat the blood and then retransfuse it instead of, or in addition to, donor blood (allogeneic transfusion).
Autotransfusion is recommended for hemorrhagic or high-risk hemorrhagic surgeries, such as cardiac, vascular, trauma, orthopedic, kidney or liver transplants and some neurosurgeries.
The limitations
of centrifugal autotransfusion
However, current autotransfusion machines only allow the patient’s red blood cells to be saved. This is an important limitation since it means that transfusions of donor platelets are still needed if the bleeding is too massive.
- Loss of patient platelets
- In case of massive bleeding, need for platelets
- Cost of multiple transfusions
- Complex equipment, steep learning curve
